IT TAKES A VILLAGE… OR MAYBE A LOTTERY: CONTEXTUALIZING COVID-19 VACCINE HESITANCY AMONG BLACK AMERICANS
[➡︎ read the rest of the symposium | watch the conference video]
Maliha Sarwar*
Abstract
As the COVID-19 vaccine rollout becomes more widespread in the United States, a large group appears to be left out. Black Americans are being vaccinated at half the rate of white Americans, despite the fact that they have been disproportionately harmed by the coronavirus and accompanying policy responses. A closer investigation into this issue is necessary to reveal the source of this hesitancy. Years of mistreatment in the medical system has led to integrational trauma, and this mistreatment has continued in the form of inaccessible and inequitable vaccine distribution. Furthermore, much of the mobilization targeting this gap in vaccination is from community leaders rather than state officials, bolstering the sentiment that racialized communities are on their own in this pandemic.
“I do not want to be killed by a white doctor in America. I think I will be killed by a white doctor in America” (Laymon 2021, 33).
Kiese Laymon, a Black author from Mississippi, describes his experience growing up in America, and the belief system that comes with it. A white doctor has the power to kill you or save your life, and your best shot is avoiding healthcare at all costs (Laymon 2021, 34). Laymon advises other Black Americans: should you have to visit a physician, dress as proper as you can, over-enunciate your English and hope and pray that it will be enough for them to look past your skin color (Laymon 2021, 35). The anxiety and mistrust reported by Laymon, and many other Black Americans, describes a phenomenon white Americans have been largely able to ignore until the rude awakening of the COVID-19 pandemic. Health care is not an apolitical experience, and care systems do not cater to all in a universal way. The standard of care and the experience of receiving it are deeply contextualized.
Health care systems have been shaped and created by white medical providers and administrators for white patients. Historically, the standard of medical care designed for and offered to Black people has been substandard, grudgingly provided, and often resulted in extreme discomfort and mistreatment for many Black patients. These effects are now more evident than ever, when being a Black American increases the likelihood of being hospitalized after contracting the coronavirus 2.9 times and doubles the likelihood of death (CDC 2021a).

The disproportionate distribution of illness associated with COVID infection in Black communities is compounded by the low rate of vaccination. Both the disproportionate access to healthcare and the failure to understand the societal factors that create mistrust are linked to systems of institutional racism. It is only when these historical trends are examined that the low vaccination rates in Black communities can be understood. The combination of a history of poor experiences within the medical system, and a lack of access to proper healthcare may be leading some Black Americans to feel remaining unvaccinated is a safer choice (Khubchandani and Macias 2021, 2). An analysis of the discourse and ethnography of Black community leaders, and the social determinants of health that affect them, demonstrates that even before the COVID-19 pandemic Black Americans experienced dangerously inadequate health care in the United States. In this paper I will examine how the American healthcare system has continued to let down Black Americans for generations, culminating in the shocking racial disparity in health outcomes amid the current COVID-19 pandemic. Even now attempts to increase vaccination rates in these populations demonstrates a lack of connecting and understanding vulnerable groups.
When it is a matter of life or death, there is no time to wait for the government to come and support you. Across the southern United States, Black community leaders have been mobilizing whatever resources are at their disposal to combat the structural violence they are faced with. They are doing all they can to get their communities vaccinated (Jacobs 2021b). In Louisiana, where 32% of the population is African American and only 23% have been vaccinated, Cala Brown, a nurse in Baton Rouge is working hard to get the word out that vaccination is essential in fighting COVID (Jacobs 2021b). “At your age, it’s the vaccine or the grave,” she states soberly as she reaches out to anyone she knows who may be feeling skeptical (Jacobs 2021b). Although a passionate believer in vaccination, she must come to terms with the fact that many of her peers can recount histories of abuse at the hands of the American medical system (Jacobs 2021b). She does her best to acknowledge this intergenerational trauma, as for many, this mistrust in the system is the root of hesitancy in accessing vaccines. She believes that it is only by acknowledging the past do we have a chance and shaping a better future (Jacobs 2021b).
Next door, in Tuskegee, Alabama, the infamous Syphilis study was conducted in 1932. Without their consent, six hundred Black men, many with syphilis, were studied and prevented from accessing treatment for the disease (CDC 2021b).

In 1997, the Clinton Administration issued an apology for the study, and the subsequent denial of treatment, with a promise to rebuild a nation where all feel safe utilizing medical systems (Clinton 1997). One of the key statements reads:
“We cannot be one America when a whole segment of our nation has no trust in America. An apology is the first step, and we take it with a commitment to rebuild that broken trust” (Clinton 1997).
Twenty-four years later, these claims appear to be no more than an empty promise. Men like Kiese Laymon continue to learn from experience that it is better to be sick at home than to leave the house and visit a doctor. This fear of harm at the hands of a medical practitioner is not to be confused with denial of science and should not be grouped as such, illustrated through the following quote: “it’s not the science we distrust; it’s the scientists” (Hoffman 2021). So, what is it that these scientists are doing that makes an individual hesitant to be vaccinated, despite the fact that they may be at higher risk for serious illness?
To understand this, one must turn to the social determinants impacting the health of Black populations in America, and how this has shaped their experiences of care. The imperial nature of the construction of the United States of America has left many to suffer at the hands of the state due to multitudes of intergenerational socioeconomic barriers. Black Americans are infected by COVID-19 at much higher rates than their white counterparts (CDC 2021a). General health may be lower for African Americans due to this population being more likely to work lower paying front line jobs and live in overcrowded housing that prevents distancing from sick individuals, and being less likely to have access to medical services nearby and the impact of wealth and educational gaps (CDC 2021a). All these are factors in the spread of disease during the current pandemic. This susceptibility to illness is created by structural barriers, not genetic differences (Bell et al. 2019, 224). However, recent efforts to provide preventative care to offset these factors have often been driven by an incorrect conflation of race and genetics. This, in turn fuels further racism, leading to a medical perception that dark skin is inherently linked to being unable to take care of oneself (Bell et al. 2019, 226).
The harmful internalization of racist medical theories has led 80% of African Americans to believe that the diet linked to their culture was the reason for their illness as opposed to all the other factors that may contribute to an unhealthy lifestyle (Bell et. al 2019, 228). As a result, physicians have often attempted to “teach” patients how to live “better” lives, that will “tease” out traditional practices (Bell et al. 2019, 231). Despite promises to create further trust in these systems as stated in the Clinton apology, 79% of clinicians claimed a person’s race would impact the treatment they gave them (Bell et al. 2019, 230).
On top of creating mistrust, stereotyping can also lead to Black patients being misdiagnosed (Acquaviva and Mintz 2010, 703). A young girl named Lela entered the hospital at age four and was diagnosed as “just another black girl with a fever and a cough” (Acquaviva and Mintz 2010, 704). Finally, years later, a radiologist who had only seen her chest scan asked, “who’s the kid with cystic fibrosis?” (Acquaviva and Mintz 2010, 704). The profiling and dismissal experienced by Lela could have cost her life. Rather than addressing the structural violence that leads to racialized individuals being more affected by an illness, many dominant medical systems instead place the blame on the patient. Uncomfortable subject positions begin to form where a doctor is now an all-knowing power educating a Black person who is assumed to be unable to take care of themselves, and in Lela’s case, dismissing and invalidating a patient’s concerns, perhaps even deeming them an overreaction.
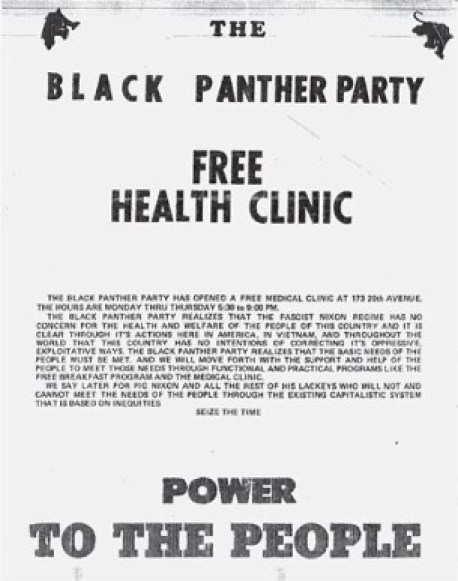
The experience of belittlement and mistreatment from being automatically labeled as a vector for disease has led some to turn to community-based initiatives. In the 1970s in Chicago, and other cities, the Black Panthers started their own free health care clinics to allow members of their communities to access medicine and combat the structural inequalities that prevented Black communities from using mainstream sources (Jerome 2019, 540). The clinics they established in Chicago offered, for some, their first visit to a healthcare facility providing both a sense of agency and an opportunity for education. However, they were quickly shut down by the Chicago board of health for alleged violations (Jerome 2019, 541). These clinics could have been used as a site for collaboration between community leaders and state officials, but instead became yet another way for Black populations to be neglected by healthcare systems.
In 2021, as the COVID-19 vaccine rollout takes place across the United States, community-based mobilization appears to be one approach that is contributing in a big way to what is getting shots in the arms of Black people in Louisiana (Jacobs 2021b). Vaccine clinics are located in predominantly white areas, providing a major logistical challenge for those lacking transportation, or working essential jobs that prevent them from taking time off work (Jacobs 2021b). This provides some insight as to why African Americans are being vaccinated at half the rate of white Americans despite them being much more affected by the pandemic (Jacobs 2021b). Ms. Brown has been working with the East Baton Rouge Council on Aging to provide vans for individuals attempting to seek vaccination but lacking transport (Jacobs 2021b). As she goes door to door, she appeals to elders that have authority in the community reminding them of their role to encourage others to get vaccinated (Jacobs 2021b).

There is often a disconnect between the reasons community workers cite for low vaccination uptake and the state-based strategies adopted to try and increase vaccination rates. Although New York Times reports coming out of communities in Louisiana critique the location of clinics and need for cell phone or internet service to book an appointment, the Louisiana government has chosen a different approach to appeal to those who are not yet vaccinated. The “Shot at a Million” program is offering multiple lotteries draws of up to one million dollars to American citizens not convicted of felonies who have received a shot (Shot at a Million 2021). The money to fund this has been taken from the Federal Coronavirus Relief Funds (Shot at a Million 2021). Once a winner has been selected for one of the draws, the money will first go back to the State of Louisiana to recoup any debts owed (Shot at a Million 2021). This is not the only “innovative” attempt the state has used to try and increase vaccine uptake. The Governor took to popular social media app “TikTok” to boast about the state’s “shot for shot” program letting eligible participants receive a free alcoholic beverage at participating bars once vaccinated (AP News 2021).
These attempts to appeal to the unvaccinated population fail to recognize the multitude of structural factors that are keeping them from being vaccinated. Many within Black communities do have trust in family doctors and community leaders, just not the state which has a history of neglecting basic needs and failing to provide access to clinics (McLernon 2021). State officials should be attempting to collaborate with Black Americans like Nurse Brown, to examine the exclusionary system that is holding back the state in vaccination numbers (Sobo et. al 2020, 246). The programs set up in Louisiana that still neglect the needs of its Black citizens is yet another painful reminder of the failure of American healthcare when it comes to adapting to serve diverse populations.
These struggles with vaccine accessibility are not unique to Louisiana. In Alabama, a state that does not even require vaccine providers to collect data on race Black Americans are being forced to advocate for themselves (Jacobs 2021a). A community leader states, “we’ve got to fend for ourselves because no one else is going to help us. That’s the way it’s always been for poor Black people living in the country” (Jacobs 2021a). Just like in many other communities, the barriers regarding internet coverage and transportation make it difficult to secure appointments, but residents here do not feel like they have a palace to turn to in order to seek help. It is almost an understanding that comes with being a poor Black person living in America. The system is not there to protect and look after you.
Although many Black citizens are working the frontlines keeping the country running, the system does not value them as such. On top of surviving in a global pandemic, they also deal with the added pressure of taking time off work to advocate for their neighbors or register and drive them themselves. The state of Alabama has not made it easy to make do for anyone, as rejection of Medicaid expansion under the affordable care act and budget cuts leading to a 35% staffing reduction seem to be staking odds against people in the state (Jacobs 2021a). With this state mandated destruction of resources and infrastructure there is very little wiggle room left for anyone that may struggle with accessibility issues or lacking the privilege to bypass them.
Where the state appears to be lacking in appealing to racial disparities of vaccine uptakes, some family doctors seem to have a better understanding of what is making people hesitant. The Cahaba Community health centers in central Alabama have produced a number of COVID-19 FAQ videos stating that the vaccine will be safe for any individual regardless of race and ethnicity, trying to ease skepticism, using whatever trust or influence they have to encourage people to get vaccinated (Cahaba Medical Care, 2021). Hearing these words from a familiar face as opposed to governmental systems that present themselves with many unknowns shrouded in medical jargon, will hopefully provide the state with the results they need to see. This demonstrates the level of understanding that family doctors have, as they realize fears of medical racism are what are preventing their patients from seeking the vaccine, not the lack of a grand prize lottery.
Regardless of the effect this has however, family doctors cannot magically make vaccination sites occur in the neighborhoods that are being neglected, and they cannot provide their patients with a home phone and internet access needed to book appointments, nor the vehicles to get them there. Though their work may be helpful, it is only when mass mobilization comes from officials that numbers will rise.
The so-called “trusting” relationships that the American government has claimed to rebuild with Black citizens has neglected the implications of the historical trauma they themselves have caused. Although they may attempt to move past it, the intergenerational wounds that have come from it are ever present in the face of the COVID-19 pandemic, when survival depends on blindly following people such as Dr. Fauci under the assumption that they have your best interests in mind and will look out for you. Black Americans will not frequent establishments and institutions they believe will cause them more harm than good, especially while the vaccination rates remain so low in their own communities, stopping them from seeing any positive outcomes of the shot.
The utilization of preventative care to try to mitigate health risks among vulnerable communities has created even more structural racism in medical institutions, justified as genetic trends. This neglects the situations members of different races have been forced into as a result of discrimination. The harmful narrative it produces, by constantly painting Black Americans as lesser, removes the blame from the institutions that should be working to remedy the issues like lack of access to basic health care clinics. The American government, and individual state governments need to start listening to and uplifting Black voices. These communities know what they need and what is stopping them from getting vaccinated. Leaders like Cala Brown in Baton Rouge, Louisiana are doing phenomenal work that needs to be supported and backed by the state. However, this work should not have been left to them. It is the responsibility of a government to take care of its people, not provide them with gimmick lotteries to push vaccination. The COVID-19 pandemic has starkly pointed out the racial issues in health care systems, and it is time to listen to stories that are being shared to finally address the roots of problems plaguing the nation, so lasting trust may finally be rebuilt.
Works Cited
Acquaviva, Kimberly D., and Matthew Mintz. “Perspective: Are We Teaching Racial Profiling? The Dangers of Subjective Determinations of Race and Ethnicity in Case Presentations.” Academic Medicine 85, no. 4 (April 2010): 702-05. doi:10.1097/acm.0b013e3181d296c7.
Bell, Hannah S., Funmi Odumosu, Anna C. Martinez-Hume, Heather A. Howard, and Linda M. Hunt. “Racialized Risk in Clinical Care: Clinician Vigilance and Patient Responsibility.” Medical Anthropology 38, no. 3 (2019): 224-38. Accessed 2021. doi:10.1080/01459740.2018.1476508.
Black Heritage Society of Washington State, The Black Panther Party Free Health Clinic (Seattle, 1971).
a “CDC COVID Data Tracker.” Centers for Disease Control and Prevention. Accessed June 06, 2021. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic.
Clinton, Bill. “Apology For Study Done in Tuskegee.” Speech, The East Room, The White House, Washington, D.C., May 16, 1997. Accessed 2021. https://clintonwhitehouse4.archives.gov/textonly/New/Remarks/Fri/19970516-898.html.
Hoffman, Jan. “‘I Won’t Be Used as a Guinea Pig for White People.” The New York Times. October 07, 2020. Accessed June 28, 2021. https://www.nytimes.com/2020/10/07/health/coronavirus-vaccine-trials-african-americans.html.
John Waits. “COVID-19 Vaccine FAQ”. Cahaba Medical Care, YouTube, (April 29, 2021).
Jerome, Jessica. “Much More than a Clinic: Chicago’s Free Health Centers 1968-1972.” Medical Anthropology 38, no. 6 (2019): 537-50. doi:10.1080/01459740.2019.1633641.
a Jacobs, Andrew. “All Hands on Deck’: When Vaccinating Black People Is a Communal Effort.” The New York Times. March 28, 2021. Accessed 2021. https://www.nytimes.com/2021/03/28/health/covid-19-vaccine-african-americans.html.
b Jacobs, Andrew. “‘At Your Age, It’s the Vaccine or the Grave’.” The New York Times. March 06, 2021. Accessed 2021. https://www.nytimes.com/2021/03/06/health/african-americans-vaccine-hesistancy.html.
Khubchandani, Jagdish, and Yilda Macias. “COVID-19 Vaccination Hesitancy in Hispanics and African-Americans: A Review and Recommendations for Practice.” Brain, Behavior, & Immunity – Health 15 (May 21, 2021). doi:10.1016/j.bbih.2021.100277.
Laymon, Kiese, “My Head is a Part of my Body and Other Notes on Crazy,” in You are Your Best Thing, ed. Tarana Burke and Brene Brown (New York, 2021), 33-42.
“Louisiana: Statewide Shot for a Shot Vaccine Campaign.” American Press News. May 27, 2021. Accessed 2021. https://apnews.com/article/la-state-wire-louisiana-lifestyle-business-coronavirus-pandemic-fd30aec9fa10e761d2628c9105c216cf.
McLernon, Lianna. “Experts Seek to Allay COVID Vaccine Hesitancy in Black Americans.” Center for Infectious Disease Research and Policy. February 09, 2021. Accessed 2021. https://www.cidrap.umn.edu/news-perspective/2021/02/experts-seek-allay-covid-vaccine-hesitancy-black-americans.
Records of the Centers for Disease Control and Prevention, Record Group 422, Tuskegee Syphilis Study, 1932-1972, Photographic Print, Tuskegee (Ala) https://www.archives.gov/atlanta/exhibits/item470-tag.html
Shot At a Million. 2021. https://shotatamillion.com/.
Sobo, E. J., Helen Lambert, and Corliss D. Heath. “More than a Teachable Moment: Black Lives Matter.” Anthropology & Medicine 27, no. 3 (July 2020): 243-48. doi:10.1080/13648470.2020.1783054.
b “Tuskegee Study – Timeline – CDC – NCHHSTP.” Centers for Disease Control and Prevention. April 22, 2021. Accessed 2021.
Records of the Centers for Disease Control and Prevention, Record Group 422, Tuskegee Syphilis Study, 1932-1972, Photographic Print, Tuskegee (Ala). https://www.archives.gov/atlanta/exhibits/item470-tag.html
Ruth Talbot and Sean McMinn, Where COVID-19 Vaccination Site are in East Baton Rouge Parish, February 4th, 2021, Map, Louisiana Department of Health, Census Bureau.
* Maliha Sarwar (she/her) is pursuing a double major at the University of Toronto in Sociocultural Anthropology and History. Her presentation at the Ethics Intersections Reflections conference examines institutional medical racism in the United States, and its impact on COVID-19 vaccine uptake in Black Americans. Through her research she hopes to shed light on the importance of working directly with communities to better understand intergenerational medical trauma and create long term solutions for a more equitable future. Maliha is incredibly interested in the intersection of ethics and policy and enjoys examining contemporary global issues through a historical lens. When she’s not working, Maliha loves to take long walks through Toronto and explore new parts of the city.


You must be logged in to post a comment.